One approach stands out in the pursuit of effective treatment for atrial fibrillation: electrical
cardioversion. This comprehensive guide delves into cardioversion’s pivotal role in managing fibrillation. We
will explore the intricacies of this procedure, its potential benefits, considerations, and expected
outcomes.
Understanding Atrial Fibrillation
Atrial fibrillation is among the most prevalent heart rhythm disorders affecting millions worldwide. Atrial
fibrillation (AF or AFib) is an arrhythmia where a patient experiences abnormal heartbeats. These irregular
heartbeats can come in the form of a faster pattern than the normal level. Normally, the upper chambers of the
heart, called atria, contract in a coordinated manner, and the lower chambers, called the ventricles, follow.
However, in the case of fibrillation, the atria contract irregularly, causing the heart to lose a coordinated
course of action.
Some common symptoms of fibrillation are:
- Heart palpitations: You may feel a fluttering of rapid heart sensations.
- Fatigue: A decreased cardiac output can lead to laziness and tiredness throughout the day.
- Dizziness or lightheadedness: The blood flow to the brain may be affected, leading to dizziness or
even fainting in extreme cases. - Shortness of breath: You may feel short during routine physical exertion or exercise.
- Chest pain or discomfort: Though not as common as other symptoms, chest pain can be an important
indication of fibrillation.
There are three distinct types of fibrillation that you may experience. In Paroxysmal AF, the irregularities in
the heartbeats may return to normal heart rhythms after a short period without intervention or testing. The other
type is Persistent AF, where irregular heartbeats last longer than a week and usually do not self-terminate. The
last type is known as Permanent AF, which is in a much longer term than the other two types. Medical
intervention is required to treat Persistent and Permanent AF.
The Impact of Fibrillation on Cardiac Health
Atrial Fibrillation is more than just an irregular heart rhythm disorder. It can have significant impacts on
your cardiac health if left untreated. There is an increased risk of blood clot formation. Irregular heartbeats
can cause blood to remain stagnant and lodged in the atria. Large amounts of blood accumulation in one region
can increase the risk of blood clots.
AF is the leading cause of ischemic strokes. This occurs when a blood clot formed due to irregular heartbeats
blocks a major blood vessel supplying blood to the brain. These strokes are a severe health hazard and may have
lasting impacts on your health. Patients suffering from AF are prescribed particular medicines like
anticoagulants and blood thinners to minimize this type of risk.
The irregularity in the heart’s function can cause its abilities to be compromised in the long run. This can
seriously damage its blood-pumping function and cause the heart to weaken over time. At this stage, you may feel
symptoms like shortness of breath, fluid retention, and fatigue, clear signs of fatal heart failure.
AF can worsen these issues for people with any prior cardiac conditions, such as coronary artery disease or
heart valve problems. Moreover, it can seriously impact the quality of your life. The symptoms like fatigue,
palpitations, dizziness, and shortness of breath can limit your ability to indulge in daily activities, in
addition to mental and emotional distress.
Exploring Treatment Options
There are a range of different treatment options for curing atrial fibrillation. The treatment aims to restore
a healthy heartbeat, manage symptoms, reduce the risk of complications, and enhance your quality of life. The
first-line treatment option for AF is the use of medication. They control heart rates, restore heart rhythms,
and prevent any clot formation in the blood. Some key medicinal choices often prescribed are antiarrhythmics,
anticoagulants, beta-blockers, and calcium channel blockers. They can either be prescribed in isolation or in
combination with each other, depending on your condition.
Another major treatment choice is the use of electrical cardioversion. It uses electric shocks to make the
heartbeat patterns return to normal. It’s usually used when medicinal treatment alone has not successfully
maintained a normal rhythm or when prompt rhythm correction is required. The procedure is performed under
anesthesia, and the shock synchronizes the heart’s electrical activity, making it return to a normal rhythm. The
minimal risk of the process, along with its utility, make cardioversion successful in treating AF.
Other less popular options available include procedures called catheter ablation and defibrillation. These are
generally less invasive treatment methods that have proven successful over time. In addition to these, certain
lifestyle modifications can impact AF management. By reducing your intake of caffeine and alcohol, as well as
adopting a heart-healthy diet, you can aim to manage AF. Adopting exercise and physical activity into your
routine can also help manage AF symptoms.
What Is Electrical Cardioversion, and How Does It Work?
Cardioversion is a medical process by which a range of heart disorders are treated. These heart conditions
cause the heart to beat faster or with irregularity. The cardioversion procedure delivers controlled electric
signals to the heart to regulate the heartbeats. While the thought of an electrical shock to the heart may sound
intimidating, cardioversion is a safe and well-established medical intervention trained healthcare professionals
perform.
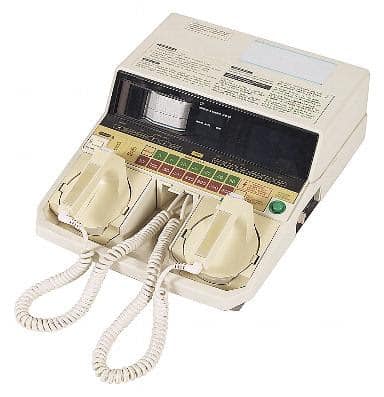
Cardioversion requires specialized equipment that delivers controlled electrical impulses to the heart. These
shocks disrupt the malfunctioning electric signals emitted by the heart and “reset” the heart’s electrical
system. The result is a return to regular heart rhythms. This procedure can restore the heartbeat pattern to the
normal level almost instantly, without a delay. Here’s what to expect when going for this type of
treatment:
- Before the procedure, you’ll undergo a thorough testing and evaluation process, including an assessment of
your overall health, an electrocardiogram (ECG or EKG) to record your heart’s electrical activity, and a
discussion of anesthesia options.
- You may receive anesthesia or sedation to ensure your comfort during the procedure. The level of
anesthesia depends on your specific case and the doctor’s recommendations. - Special electrode pads are placed on your chest. These pads are connected to a cardioversion machine,
which delivers the controlled electrical shock. - Once you are prepared and under anesthesia, the specialized doctor delivers an accurately timed electrical
shock through the electrode pads. This shock “resets” the heart’s electrical signals, hopefully restoring a
normal rhythm.
- Throughout the procedure, your vital signs, including heart rate, rhythm, blood pressure, and oxygen
levels, are closely monitored to ensure your safety.
Choosing Between Electrical Cardioversion and Other Treatment Options
- Cardioversion vs. Medication Treatment: As explained above, medicines are usually the first
treatment option that doctors consider to treat AF. However, sometimes, it is seen that the patient’s
condition is beyond the scope of medication treatment. In this case, the cardioversion recovery method is
imminent. Moreover, medications used to control AF can have unwanted side effects, such as fatigue,
dizziness, or gastrointestinal issues. - Cardioversion vs. Ablation: Catheter ablation is a minimally invasive medical process that is used
to treat AF. Under this procedure, a catheter is inserted intravenously into your blood vessels. It uses
radio-frequency energy or freezing techniques to specifically target the malfunctioning heart tissue to stop
the arrhythmia. However, ablation is an effective treatment only for certain types of atrial fibrillation.
Not all patients are suitable candidates for this type of treatment. Some may have contraindications or
anatomical factors that make them less ideal candidates. In such cases, electrical cardioversion may be the
better option. - Electrical Cardioversion vs. Defibrillation: Defibrillation is a medical procedure to treat fatal
ventricular arrhythmias, specifically ventricular fibrillation and pulseless ventricular tachycardia. It
achieves this differently than cardioversion. Defibrillation operates on the principle that electric shocks
to the heart will halt any cardiac activity. It is assumed that when the heart starts to beat again, it will
do so with the regular rhythm. However, it is used mostly in extreme cases and emergency situations.
Side Effects of Cardioversion
Cardioversion is generally considered a safe and effective process. However, as is the case with any medical
procedure, cardioversion has some risks and side effects that you must discuss with your doctor before opting to
undergo the procedure. The most common one that the majority of people face is pain and discomfort during the
procedure. This is generally felt in case there is a weaker administration of anesthesia or sedation and the
patient is slightly conscious. However, aside from the slight discomfort, this is usually not dangerous for the
patient.
The electrode pads attached during the process may impact your skin. They can cause irritation or redness while
being attached to your chest; however, this is not a long-lasting condition and will heal itself after the pads
are removed. It would help if you communicate any skin-related conditions to your doctor before they attach the
electrode pads.
Sometimes, anesthesia and sedation can cause vomiting and a nauseating feeling among the patients. These side
effects usually subside as the effects of the anesthesia wear off. Moreover, there is an increased risk of clot
formation in the atria. These clots already exist in the system; with cardioversion, there is a chance of them
being dislodged. This could result in fatal conditions like stroke or other embolic conditions. Anticoagulant
medications are often prescribed before cardioversion to counter this.
Success Rates
The success rates and the expected outcomes of electric cardioversion depend on various factors. These include
the underlying heart condition, the timing of the procedure, and patient-specific factors. The chances of
success are higher if cardioversion is done promptly after arrhythmia diagnosis. These changes may also be
affected by pre-existing conditions that you may have, as they complicate the recovery process. In this case,
there may be a need for cardioversion to be done repeatedly on multiple occasions. The use of medications before
and after cardioversion can increase the chances of success and can reduce the risk of arrhythmia recurrence. It
is best to consult a doctor
for further information regarding your own condition.
Conclusion
In cardiac and heart care, electrical cardioversion is a valuable tool for restoring regular cardiac rhythm and
improving the quality of life for individuals dealing with fibrillation (AF) and related arrhythmias. This
procedure, while not without considerations and potential risks, offers hope and immediate relief to
many.